

About Brandon M. Welch, MS, PhD, Founder & CEO
Brandon M. Welch, MS, PhD, is an NIH-funded researcher, innovator, and entrepreneur dedicated to creating the future of healthcare through user-friendly health technology.
Dr. Welch is the founder and CEO of doxy.me, a leading telemedicine software company used by over 1 million providers in 176 countries. Notably, doxy.me emerged as a leading telehealth solution during the pandemic, facilitating 8 billion+ minutes of care.
In his recent book, “Telehealth Success: How to Thrive in the New Age of Remote Care,” Dr. Welch offers invaluable insights into what it takes for clinicians and healthcare organizations to be successful with telehealth.
Dr. Welch holds a Masters of Science in Human Genetics from Tulane University and a PhD in Biomedical Informatics from the University of Utah. Additionally, he is an associate professor at the Medical University of South Carolina, where he has authored multiple peer-reviewed articles.
Dr. Welch enjoys spending time with his family in Charleston, SC.

About doxy.me
Doxy.me is the world’s most loved telemedicine solution. Founded in 2014 by Dr. Brandon Welch, doxy.me enables healthcare organizations to provide virtual care that’s accessible to everyone, everywhere, on any device. According to KLAS research, doxy.me is the number one telehealth solution healthcare organizations relied on during the COVID-19 crisis. Doxy.me has facilitated nearly 9 billion minutes of telemedicine in over 176 countries. Doxy.me is HIPAA compliant, works in-browser, and requires no downloads. To learn more, visit doxy.me.
Medical Travel & Digital Health News (MTDHN): Tell us about yourself and how you got started with doxy.me.
Brandon Welch (BW): I developed an interest in healthcare in high school where I first learned about genetics and its application in diagnosing and treating diseases. This initial exposure ignited my passion for healthcare medicine, leading me to earn a master’s degree in Human Genetics.
Through genetics, I was introduced to the concept of using digital health, technology and computers to help manage genetic information. I went on to earn my PhD in Biomedical Informatics from the University of Utah to obtain the tools needed to build the health IT systems, therefore supporting genetics in medicine. Essentially, the work around my PhD surrounded the use of computers to help doctors use genetics, which is something I’m very passionate about.
While pursuing my PhD, I also worked on several side projects. One of the projects was for the community in Utah and aimed to address challenges faced by women in rural areas, particularly regarding prenatal care access. In rural communities, women often had to travel long distances for routine prenatal checkups, which seemed unnecessary. This led us to explore telemedicine solutions to provide high-quality prenatal care remotely.
We were looking at ways to provide high quality prenatal care without requiring patients to travel. This was back ten years ago when telemedicine was just starting to emerge and people were investigating its value.
At the time, Skype and FaceTime were popular so we thought that telemedicine using these platforms would be a good idea for our project. However, we hit a wall when we were not given permission to use these platforms because they were not HIPAA-compliant. This led me to think about using HIPAA-compliant telemedicine solutions but I saw that there weren’t very many in existence and the ones that were available were expensive and complicated.
I remember thinking at the time, “Where’s the simple and free telemedicine solution? Everything on the Internet is free – why isn’t there a free telemedicine solution?” I even went to Google and typed in “simple and free telemedicine software,” and nothing came up!
I couldn’t believe that no one had built a free telemedicine app.
Since I was a student at the time, my friend and I decided to enter one of the student innovation and idea competitions and submitted our idea. We ended up winning the Consumers Choice award and we took the prize money to build the first prototype of a simple and free telemedicine app, now known as doxy.me.
MTDHN: What is your role within the company?
BW: As one of the founders, I play a pivotal role in steering the direction of the company. As an innovator and professor, I am constantly generating ideas and contributing to design discussions to optimize the platform for both providers and patients.
I’m deeply involved in day-to-day operations and a large part of my focus is on charting the company’s future course. I look out to see where we’re at now and look out to the future to plot our course for potential challenges and opportunities – you can say I’m the captain of the ship, constantly scanning the horizon for other icebergs and ships.

MTDHN: What was the growth process like for Doxy.me?
BW: Doxy.me experienced natural, organic growth from its launch in 2014 until the onset of COVID-19 in 2020. Initially, we had about 80,000, which is a good user base. Then during the pandemic, the demand for telemedicine surged dramatically.
Within two months, our user base skyrocketed to 700,000 users and we now serve approximately 1.5 million healthcare providers, conducting about 9 billion minutes of telemedicine since the pandemic began.
MTDHN: What is your business model?
BW: Doxy.me is a software service where providers pay a monthly fee to use it. It’s $30 a month for a professional account but we also have a free version where you get to sign up and use it at no cost.
However, for the professional version, you get additional tools that you can use during the call, such as collecting payments, screen share, group calling, notification alerts and other features that providers like to use. So, we’ll often see them upgrade to the professional version.
We also have a clinic version designed for hospitals, health systems and/or clinics with multiple providers. In this version, you get a sub-domain which would look like: [Your Hospital Name].doxy.me. You get your own branding, which is important to many health organizations that they get their logo, colors and name in the URL. That’s why a lot of health systems, hospitals and clinics like to go with this version because it’s more personalized and branded for them.
MTDHN: Can you expand more on your provider base? Who are they?
BW: About 60-65% of our providers are mental and behavioral health specialists such as counselors, therapists, psychiatrists, psychologists, social workers, etc. They are the ones that have hour-long sessions because it works very well for their patient base since they don’t have to travel and the time is used for more talking.
The remaining 35-40% are your traditional physicians, primary care doctors, pediatricians as well as 100 other specialties, such as dermatology and cardiology.
MTDHN: Are there any remote patient monitoring capabilities?
BW: While we do not directly offer remote patient monitoring capabilities, we partner with companies that provide such services.
For example, the echo stethoscope and its software can run parallel to doxy.me. On a video call, the physician can have the patient put it up to his/her heart and it will transmit through the software that they use with our program. However, it’s not necessarily integrated into doxy.me.
There is also the otoscope which the physicians can use to look into the ear or mouth that will run through doxy.me. It is a USB which they can simply connect to their computer and then change from the normal camera to the otoscope camera.
MTDHN: What do you think differentiates doxy.me from the hundreds of other telemedicine companies out there?
BW: The thing that we hear often from our providers is that they love how simple Doxy.me is, which is important because healthcare can often be complicated for both providers and patients. I believe we’ve done an incredible job of keeping it simple with doxy.me.
Each provider has his/her own room, which is their own unique link that they send to their patients. The patients don’t have to download anything—they don’t have to create an account or remember passwords. All they simply do is click that link and it takes them to the room where they check in, type their name and enter the doxy.me waiting room. Then the provider starts the call — and they love it because they never have any issues with it.
We receive this positive feedback from a lot of providers. Even patients who find out that I work for doxy.me let me know that they use it with their provider and they love it, too.
I believe our simplicity resonates in healthcare because health providers are often required to use electronic health records (EHRs) which is not synonymous with simplicity. In fact, it is often a source of frustration for providers. However, with doxy.me, it is so simple it’s like a breath of fresh air.
In addition, we have a Net Promoter Score (NPS) that measures customer satisfaction and we score 60, which is up there with Amazon and Apple.
We pride ourselves in our simplicity and ease of use while also being free and low cost. We have a free version that many of our users use which is a great way to introduce them to telemedicine without the risk of paying money and not knowing how often they will even use it.
MTDHN: Are you connected at all to any health plans, employers or payers? Or is it strictly provider driven?
BW: We are strictly provider driven because we don’t have direct relationships with the patients. The health plans have the relationship with the patients and our relationship is with the providers.
We did have discussions with health plans, but their business model and ours don’t really intersect.
It’s up to the providers to decide if they want to use doxy.me and if it works well for them, the health plans then support and fund.
MTDHN: How do the providers bill for the consult? Do they bill strictly off of what their health plan is or what their typical Medicare plus billing is?
BW: It depends. The billing is the same as it is in person. The only change is that for some health plans, you sometimes do have to put a modifier in there and say, “I did this consult, but it was a telemedicine visit.” Some health plans will pay at the same rate as an in-person encounter or a little less for others. But as long as you put that modifier in there, the billing is the same.
Many mental health providers are cash pay anyway so they charge patients directly and it doesn’t involve the health plan.
MTDHN: How do you see yourself scaling this even further?
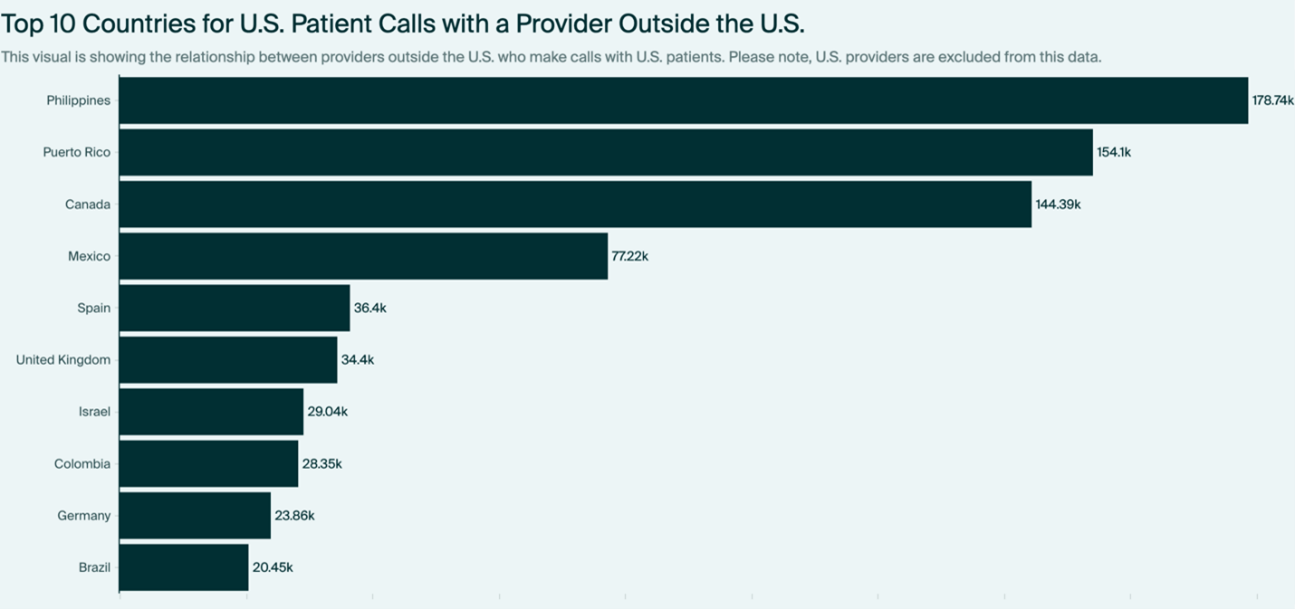
BW: We see a huge potential to scale doxy.me internationally. Currently, about 85-90% of our users are in the U.S. so we’re very U.S. centric, but we do have 10-15% outside of the U.S., which tells us that we have an opportunity in the market.
We have doxy.me translated into over 100 languages. You can have a patient who speaks Bengali checking in and they would see everything in their native language. For providers, we have about 20 languages.
Many people internationally use messaging apps such as WhatsApp or others that aren’t really designed for healthcare and are probably less secure. Therefore, we want to get the word out and let them know that, yes, WhatsApp is free, but there is also a free telemedicine app specifically designed for healthcare that is secure and better for the patient experience.
We also plan to improve our video call and add features to enhance the provider experience. For example, we’re currently testing using AI to transcribe a call and from that transcription, creating a SOAP note or a brief summary of that call, so that providers can simply copy and paste it into their EHR without having to retype everything.
MTDHN: Can you share with us which parts of the world interest you the most?
BW: We recently welcomed a new Chief Medical Officer, Dr. Esteban Lopez, who holds dual Mexican and U.S. citizenship and brings extensive experience as a medical doctor. He previously worked with Google to expand the Google Cloud in Latin America which is the region where we’ll likely concentrate our efforts first.
We’ve already established a strong presence in English-speaking countries such as Canada, Australia and New Zealand. In fact, we’re proud to be one of the leading telemedicine platforms in these regions.
Europe is another area of focus for us, with half of our workforce based there. Specifically, we have operations in the UK, Ukraine and various other parts of Europe.
In all of these regions, our core model remains consistent, but we recognize the importance of tailoring our offerings to suit local needs. This might involve adjustments in pricing or feature sets to accommodate varying market conditions and preferences.
We’re also committed to philanthropy and making a positive impact in underserved communities affected by conflict or crisis. For example, in countries like Ukraine and Israel where there’s ongoing conflict, we offer our services free of charge. This also goes for many African countries and other regions facing similar challenges and we ensure that our platform is accessible to those who need it most, regardless of their ability to pay.
